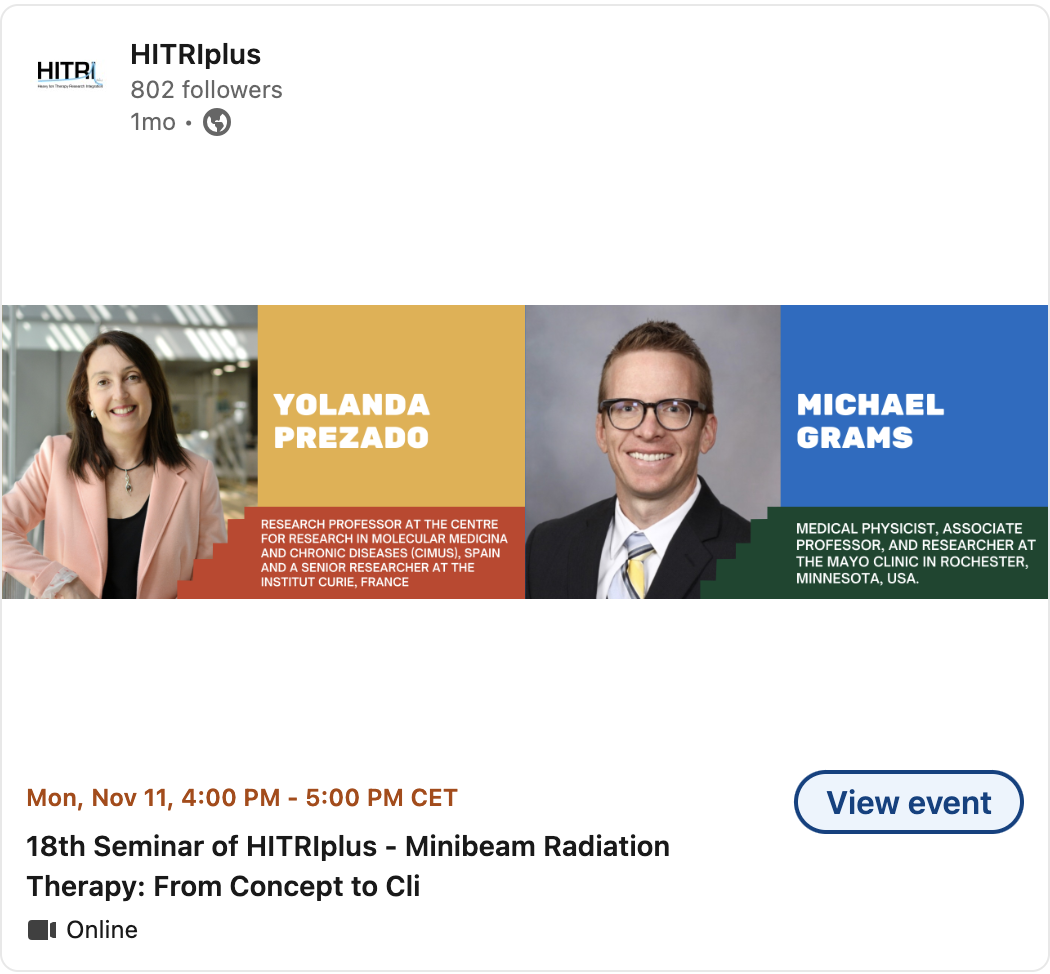
Minibeam Radiation Therapy (MBRT) with Prof. Yolanda Prezado
Q&A with Prof. Yolanda Prezado, Institut Curie
Q: In your research on minibeam radiation therapy (MBRT), you’ve explored the unique biological effects that go beyond traditional radiation therapy paradigms. What insights or unexpected results have you encountered regarding non-targeted effects, like bystander and immunological responses, in recent studies?
A: “We have observed that the immune system, particularly T cells, plays a significant role in the anti-tumor response of MBRT. Unlike conventional broad-beam radiation, where T cells remain at the tumor periphery, MBRT results in a substantial concentration of T cells in the tumor center. In fact, T cell density is notably higher in MBRT-treated areas than in non-irradiated controls or even conventional radiotherapy, observed within 48 hours post-irradiation. These findings suggest a potentially unique pathway for MBRT, which also demonstrates reduced T cell exhaustion compared to conventional approaches.”
Q: Given your role in advancing spatially fractionated radiation therapy, what key challenges or knowledge gaps need to be addressed to fully understand and optimize the potential benefits of MBRT for both tumor control and normal tissue protection?
A: “This is an exciting time for MBRT, with the first patients already successfully treated. Moving forward, I see two main research priorities to drive clinical trials: first, a deeper understanding of MBRT radiobiology at both the molecular and tissue levels, particularly the mechanisms of immune activation, vascular impact, bystander effects, and how these all influence normal tissue sparing. We need to pinpoint which biological mechanisms are dominant or interact in given applications. Second, there is a pressing need to correlate the unique dosimetry and geometry parameters of MBRT with treatment responses, as these factors differ significantly from those in conventional radiation therapy.”
Key Takeaway: “This is a blooming moment for MBRT,” Prof. Prezado shares. “We need to deepen our understanding of MBRT’s biological mechanisms and optimize its parameters to make the most of its potential in clinical settings.”
Minibeam Radiation Therapy (MBRT) with Dr. Michael Grams
Q&A with Dr. Michael Grams, Mayo Clinic
Q: As the lead physicist in Mayo Clinic’s first clinical implementation of MBRT, what were the biggest logistical and technical hurdles you faced in translating this modality from research to patient treatment?
A: “One of our main challenges was managing the relatively low dose rate of our clinical orthovoltage system, which led to long treatment times—sometimes with beam time lasting up to 15 minutes continuously. To counter potential patient movement, we attached the collimator directly to the patient, so any movement would not compromise the treatment. Our engineering team designed a solution using 3D-printed, patient-specific collimator holders, which worked as intended and allowed us to maintain a clear peak-to-valley dose differential in our minibeams, even with extended treatment times.”
Q: With MBRT now being applied in a clinical setting, how do you envision its role evolving in oncology, particularly for challenging cancer cases where conventional therapies may have limited success?
A: “I foresee MBRT initially focusing on the most challenging cases—such as re-irradiation scenarios, cases that progress despite prior treatments, and radioresistant cancers. After establishing the maximum tolerated dose in a phase 1 trial, we hope to explore its efficacy further in phase 2 trials, potentially targeting difficult-to-treat areas like head and neck or breast cancers. In parallel, we plan to advance preclinical studies to better understand MBRT’s underlying biological mechanisms, which will be crucial for maximizing its therapeutic potential.”
Key Takeaway: “I think the role of MBRT will evolve rapidly, especially for challenging cases,” Dr. Grams notes. “Expanding its clinical application will require carefully designed trials alongside continued preclinical research into its biological impact.”